I Tried Gene Therapy—and Haven’t Needed a Blood Transfusion Since!


Sickle cell disease (SCD) has long been a significant health challenge in the Black American community, disproportionately affecting individuals of African descent. This inherited blood disorder alters the shape of red blood cells, leading to painful episodes, organ damage, and a host of complications that severely impact the lives of those diagnosed. For many sickle cell warriors, the challenges of living with SCD are deeply personal and relentless, as the condition presents not only physical hardships but also emotional and social burdens.
Early Life and Sickle Cell Diagnosis
Lyric Porter’s battle with sickle cell began almost immediately after birth. Diagnosed through newborn screening, she was identified as having SS sickle cell disease, the most severe type. Her early childhood was fraught with complications, including a 14-day fever when she was just five, which left her with scar tissue in her lungs. This led to her requiring an oxygen tank in kindergarten—a sobering reality for such a young child. Throughout her childhood, Porter endured frequent health crises, including gallstones and recurrent acute chest syndrome, a life-threatening complication of SCD.
From her preteen to teenage years, Porter needed transfusions every three to four weeks. Despite this, she recognizes that her condition could have been much more severe.
“Many kids with sickle cell often have their spleens removed, but I still have mine, so I’m grateful for that. Despite several crises and hospitalizations over the years, I’ve never had a stroke,” she shares.
Porter remained determined in pursuing her academic goals, despite the health challenges she faced.
She attended Florida A&M University, where she earned her Bachelor’s degree in Broadcast Journalism in 2019. However, even during her college years, sickle cell continued to play a significant role in her life.
“While in college, I continued to experience health issues and was hospitalized frequently. After graduating, I returned to my hometown of Chicago, where I’ve received most of my care,” Porter says.
Groundbreaking Gene Therapy Treatment
Porter’s life took a significant turn when her pediatric hematologist recommended her for a clinical trial for gene therapy stem cell transplant—a groundbreaking treatment for sickle cell disease approved by the FDA last December. In 2022, Porter became the third person in the world to undergo this experimental treatment, marking a pivotal moment in her journey.
The process was complex. Doctors harvested her blood stem cells and sent them to a lab in Germany to be genetically modified. After undergoing chemotherapy, Porter’s modified stem cells were transplanted back into her body.
“It was both exciting and discouraging at times. I was the only person in Illinois and the first at my hospital to undergo the trial. The other two patients were in different states, and we weren’t connected to one another. So, there was no peer support during the process. Still, I was determined. I thought, ‘If it doesn’t work, I’ll continue living with sickle cell as I have for the last 26 years.’ I was hopeful it would improve my quality of life, and I’ve definitely seen benefits,” Porter adds.
Now, approaching her two-year post-transplant anniversary, Porter reflects on how the treatment has changed her life.
“One major change is that I no longer experience jaundice, which used to be a big conversation starter because people would notice the whites of my eyes turning yellow. I also haven’t needed any blood transfusions since the trial, and my hemoglobin levels have stabilized. They aren’t as high as an average adult’s, but they’re more consistent, usually between 9 and 11. Before the trial, my hemoglobin would drop as low as 6 or even 2, which would require urgent transfusions,” Porter says.
Although Porter continues to experience chronic pain and other complications, she has observed an overall improvement in her quality of life.
“Now, crises build up gradually, giving me some warning before things get severe. Before, I could feel fine and then, within hours, end up in the emergency room. Since the transplant, I’ve only had one hospitalization,” Porter adds.
Overcoming Challenges and Advocating for Change
Despite the improvement, Porter admits that the experience with the clinical trial was both empowering and isolating.
“Going through the trial, I often had to advocate for myself when something didn’t feel right. It’s frustrating when you’re undergoing something so groundbreaking and feel invalidated. Additionally, I had to undergo egg preservation treatments before starting chemotherapy. I wish more emphasis was placed on this aspect of care, especially for women with sickle cell, as the disease and frequent crises can affect reproductive health,” Porter shares.
For Porter, discovering that her sickle cell disease could impact her egg reserve or overall reproductive system was a discouraging revelation.
“I went into it thinking, ‘Oh, I’m only 23 or 24 at the time, they should be able to do one cycle, and I’ll meet the number of eggs they’re looking for since I’m still young.’ They told me that typically, a woman my age would average around 15 to 20 eggs in one cycle, but I was only averaging five to seven. So, I had to repeatedly undergo the shots and procedures to harvest and preserve my eggs. I had to go through it at least three or four times because I was still only getting around five to seven eggs per cycle,” Porter recalls.
Porter understands that due to the crises she experienced and the restricted blood flow to her organs, her ovaries and all aspects of her reproductive system were affected.
“No one had ever disclosed that to me before. I also know that if I hadn’t gone to Northwestern, I wouldn’t have been able to do or afford this procedure. That would have been something that scarred me for the rest of my life, having to make the decision between wanting to be healthy and wanting to be a parent in the future,” Porter notes.
As a result of this experience, Porter is driven to make this treatment more accessible to others.
One of her key concerns is the financial burden associated with such cutting-edge treatments. While her clinical trial was sponsored, some medical expenses were still billed to her insurance.
“I can’t imagine what it would be like for someone with government-assisted insurance if they were denied coverage for something so life-changing. I also hope there’s continued interest in finding curative treatments for sickle cell disease, and that healthcare providers listen to patients more closely,” Porter says.
RELATED: The Unbreakable Bond of Two Siblings Living with Sickle Cell
Message to Others with Sickle Cell Disease
For others living with sickle cell disease, especially those considering gene therapy or other treatments, Porter’s message is one of hope and encouragement. While acknowledging that gene therapy isn’t an option for everyone, she encourages patients to explore all possibilities that might improve their quality of life.
“It’s not as simple as some people think. Gene therapy and stem cell transplants require a lot of preliminary testing to determine if a patient is healthy enough for the procedure. I encourage patients to look into it and, if eligible, give it a try. It improved my quality of life, but I know it’s not an option for everyone. Some people aren’t eligible due to complications with their organs or overall health,” Porter advises.
Porter is also passionate about raising awareness about the importance of blood donations, particularly among communities of color.
“Blood transfusions were vital to my health, especially when my hemoglobin levels were low. People often overlook how important it is to donate blood, especially within the African American community. We share many antigens and antibodies, making it easier to match sickle cell patients with donors from the same background,” Porter adds. “I also learned that many African Americans have type O blood, which is a universal donor type. I always encourage people of color to donate because it can significantly improve a sickle cell patient’s quality of life. After transfusions, I always felt more energized, allowing me to do things I couldn’t when my hemoglobin was low. It’s a simple act that can have a huge impact on someone’s life.
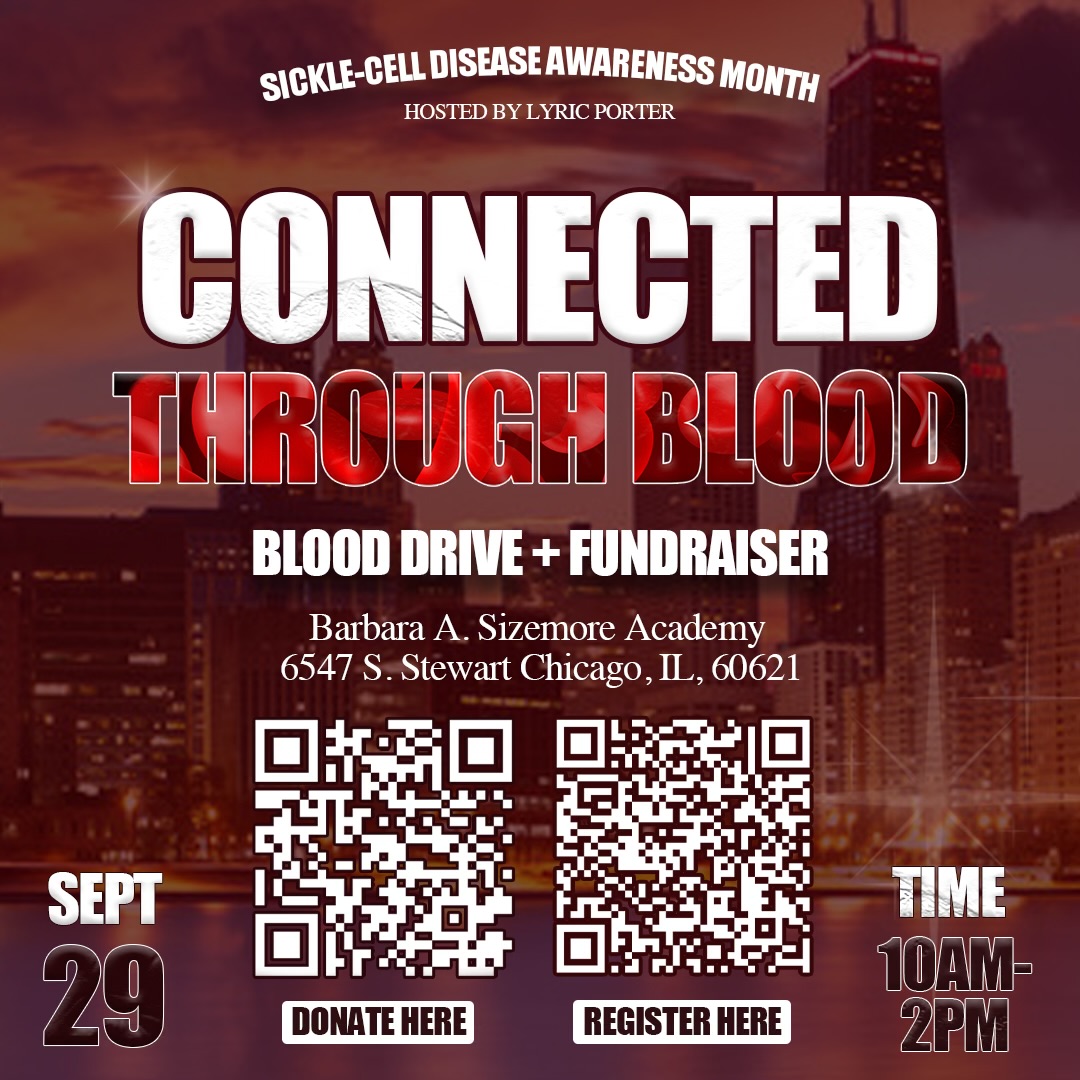
If you’re in the Chicago area and interested in donating blood, consider participating in Lyric Porter’s blood drive. See the details below.